
When stress is heightened — which it is for all of us right now because of the COVID-19 pandemic — children become aware of it and they try to locate the source of the stress. It is important to both acknowledge their concerns and be open to discussing them.
Helping children to make sense of the consequences of COVID-19 and helping them to organize their thoughts and feelings is the best approach.
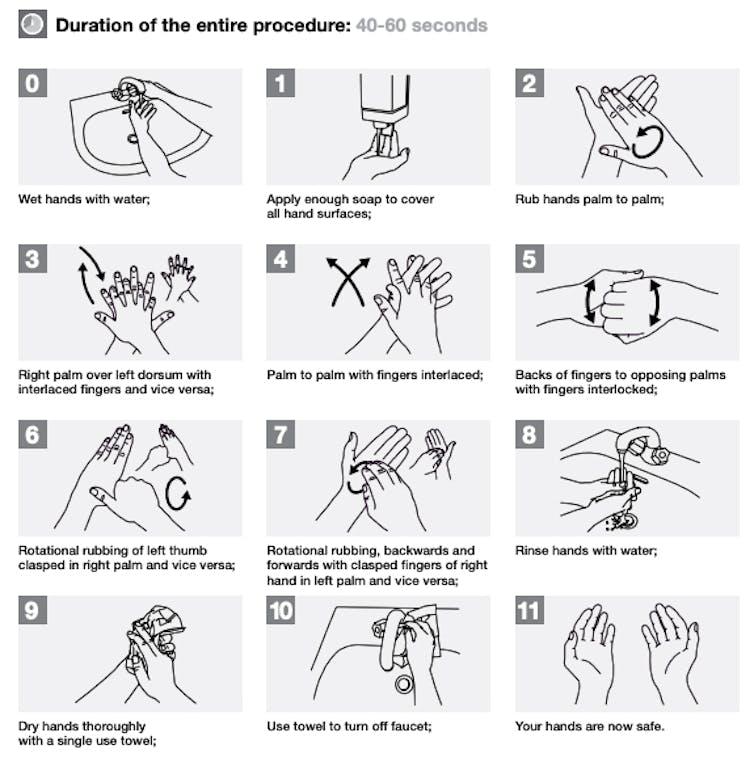
As a first step, ask your child what they know about COVID-19 or what they have heard about it. If they don’t seem too concerned, you do not need to have an in-depth conversation about it. You can simply reinforce the importance of handwashing and letting you know if they are feeling unwell.
However, if your child voices worry or concern about COVID-19, you can correct any misinformation and provide them with emotional support.
Here are some common questions parents may have about how to talk to their children about COVID-19.
Will talking about COVID-19 increase my child’s anxiety?
No, it shouldn’t. Parents often worry that talking to kids about scary social issues may increase the child’s worry and anxiety. However, it often does the opposite. As child psychologists, we often use the phrase “name it to tame it,” which means that once worries are identified and discussed (i.e. named) and a concrete coping plan is devised, worries tend to decrease versus increase (i.e. tamed). Knowledge is a powerful tool and it gives children some predictability in knowing what lies ahead, which can be very helpful in taming anxieties.
What is an appropriate age to talk to my kids about COVID-19?
It depends. First think, how well can my child manage the realities of COVID-19? The information you provide should be tailored to the individual needs of your child.
A general rule is that children’s ability to understand information about COVID-19 will be low in very young children (i.e., less than age 3) and will become more sophisticated with age. By school age, children likely have more capacity to understand and communicate what is happening. Younger children, however, can still experience the effects of stressful events in their environment.

For kids ages three to six, you might say: “There’s a germ going around, which is making people sick. We know that the best way to keep people safe from the sickness is to wash our hands a lot, and guess what, the doctors say we should sing some songs while we do that!”
For kids over the age of six, you can have a more in-depth discussion about why it’s important to wash our hands and to avoid touching our face (and the inside of our nose!). You can explain that the virus lives on surfaces that we touch (although we can’t see it) and if we touch that surface with our hands and then put our hands in our mouth or in our nose, that’s how the virus gets into our body and makes us sick, and potentially makes others around us sick (like grandma and grandpa, who can’t fight the virus as well as others).
This information can help children understand the importance of preventive measures like handwashing, as well as avoiding touching their face or putting their hands in their mouth.
Should I tell them what the symptoms are?
Yes, especially for children who are old enough to understand, such as school- aged kids. You should go through the most common symptoms of COVID-19, which include fever, dry cough, fatigue, shortness of breath, etc., and distinguish for kids how shortness of breath when they are playing a sport is different from shortness of breath when sitting down or walking around. Ask them to tell you when they feel any of these symptoms coming on. You could also tell them that you are taking everyone’s temperature morning or night, just to be safe. There is comfort for kids in knowing that parents are on top of things.
How can I help reduce my children’s anxiety and worry about COVID-19?
Here are some strategies we know work in general about anxiety and worry in kids. First, use age-appropriate language (for example, “a new germ that we don’t know very much about”), as well as coping-focused language (for example, “we are doing everything we can to keep from getting sick”), rather than language that is stress-inducing or catastrophic.
Second, avoid voicing your emotional concerns in front of your children, and be sure to monitor your own stress and anxiety levels around your children.
Third, try to avoid exposing children to background and foreground television and media reports about COVID-19. Research shows this can elevate their symptoms of stress.
Fourth, talk about your family’s plans to stay healthy such as washing hands, cancelling vacations, avoiding places with lots of people and staying home if you aren’t feeling well. You can also reassure them that very few children have been sick and if they have been, their symptoms have been mild. Children are comforted by feeling a sense of control (i.e. knowing what they can do) and by having predictability in their lives.
Lastly, as much as possible, stick to regular activities and routines for things like meals, naps, baths and bedtime. This increases predictability for kids. Spend time doing activities that promote calm in your family like reading together, watching movies, playing board games or getting outside for a walk. For younger children, you also can set up treasure hunts around the house and use play as a way to process big feelings. Children will be comforted by spending special time with you.
Are there any tips or tricks to promote handwashing?
It can be difficult to encourage children to wash their hands. Making it a habit by prompting them to wash their hands after the bathroom, before eating, coming in from outdoors, after the school day and after coughing or sneezing is a great idea. Singing a song while washing their hands can also be a great way to promote handwashing. You can also put their favourite song on the music player and dance your way through it**. If you’ve got some glitter, you can sprinkle a little bit on their hands and get them to wash it off!
What should I tell them if their daycare/school is closed, arts or sports program has been cancelled, or we have to self-isolate?
Tell them honest and factual information. You can share that this is a precaution to help slow down the spread of the germs. You can say: “Kids will be staying home because we know germs spread when there are a lot of people around. Staying home means that more people can stay healthy and will help to slow down the spread of germs.”
Any recommendations for activities to do if we have to self-isolate?
It can be helpful to maintain some of the same routines even if children are home from school. This helps children know what to expect. Having a discussion with your children about routines and expectations for the time they are home can be helpful.
Engaging in activities like reading, schoolwork, doing crafts, board games, cooking or baking with a caregiver or doing art can help the time pass. It is also important to continue getting physical activity, which can include playing outside, having an indoor dance party, an obstacle course of doing stretches/yoga.
Finally, it is important to avoid large increases in screen time because this can interfere with children’s well-being and sleep.
Although self-isolating can be stressful for parents, reassuring kids (and ourselves) that this time will pass can be helpful for keeping everyone healthy and happy.
_Other great resources for parents include information from UNICEF and the Centers for Disease Control.
Nicole Racine, Postdoctoral Research Fellow, University of Calgary and Sheri Madigan, Assistant Professor, Canada Research Chair in Determinants of Child Development, Owerko Centre at the Alberta Children’s Hospital Research Institute, University of Calgary
This article is republished from The Conversation under a Creative Commons license. Read the original article.



